Fluorosis and Renal stones
NOTE: THIS IS AN ONLINE E LOGBOOK TO DISCUSS OUR PATIENT'S DE-IDENTIFIED HEALTH DATA SHARED AFTER TAKING HIS / HER /GUARDIAN'S SIGNED INFORMED CONSENT. HERE WE DISCUSS OUR INDIVIDUAL PATIENT'S PROBLEMS THROUGH A SERIES OF INPUTS FROM THE AVAILABLE GLOBAL ONLINE COMMUNITY OF EXPERTS INTENDING TO SOLVE THOSE CLINICAL PROBLEMS WITH COLLECTIVE CURRENT BEST EVIDENCE-BASED INPUT
- Urea #58mg/dl 17 - 50
- Creatinine #3.0mg/dl 08 - 1.3
- Uric acid 6.3mg/dl 3.5 - 7.2
- Calcium #7.8mg/dl 8.6 - 10.2
- Phosphorus 2.9mg/dl 2.5 - 4.5
- Sodium 144mEq/L 136 - 145
- Potassium 3.7mEq/L 3.5 - 5.1
- Chloride 99mEq/L 98 - 107
- Hb #7.4gm/dl 13.0 - 17.0
- TC 6,900cells/cumm 4000 - 10000
- Neutrophils 65% 40 - 80
- Lymphocytes #19% 20 - 40
- Eosinophils 06% 01 - 06
- Monocytes 10% 02 - 10
- Basophils 00% 0 - 2
- PCV #23.1vol% 40 - 50
- MCV 86.8ft 83 - 101
- MCH 27.8pg 27 - 32
- MCHC 32.0 31.5 - 34.5
- RDW-CV #15.0% 11.6 - 14.0
- RDW-SD 47.9fl 39.0 - 46.0
- RBC count #2.66millions/cumm 4.5 - 5.5
- Platelet count 1.79lakhs/cu.mm 1.5 - 4.1
- 24 hrs urinary protein 454.7mg/day <150mg/day
- 24 hrs urine volume 1,800ml
- Colour Pale Yellow Pale Yellow
- Appearance Clear Clear
- Reaction Acidic 5.0 - 9.0
- SP Gravity 1.010 1.001 - 1.035
- Albumin + Negative
- Sugar Nil Negative
- Bile salts Nil Negative
- Bile Pigments Nil Negative
- Pus cells 1 - 2 0-5/HPF
- Epithelial Cells 3 - 4 0-5/HPF
- RBCs 2 - 3 0-2/HPF
- Crystals Nil Nil
- Casts Nil Nil
- Amorphous Deposits Absent Nil
- Others Nil Nil
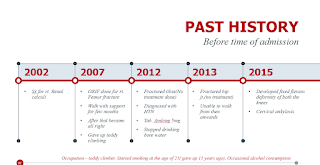
First what lead us to suspect chronic fluorosis?
Skeletal Fluorosis should be strongly suspected in any person with
features of stiffness, rigidity, restricted movements at the spine and joints,
bone and joint pains, and who has been residing continuously for >6 months in
a fluorosis-endemic area. The clinical investigations for the
confirmation of the diagnosis include the following:
- Haemoglobin%: Anaemia due to reduced erythropoietin activity secondary to fluorosis induced osteosclerosis of medullary cavities (In our patient Hb - 7.4gm/dl, RBC - 2.66 million/cumm)
- Renal function tests: These may show impaired urea clearance, decreased glomerular filtration rate, increased blood urea nitrogen (In our patient urea - 58 mg/dl)
- Radiographic features: Increased bony density(osteosclerosis) compact bone thickening, bamboo spine(ankylosing spondylitis), periosteal bone formation. ossification of the attachments of tendons, ligaments, ossification of the post. longitudinal ligament. All of which was seen in our patient.
So, how can chronic fluorosis lead to fractures?
What we learned via reviewing literature...
Vague, diffuse aches, muscle weakness,
chronic fatigue, and stiffness of joints with decreased range of motion are
common initial symptoms. These symptoms may be dismissed as
functional but may, in fact, be early signs of fluoride damage to tendinous
insertions and ligaments as well as joint capsules. During later stages, calcification of the
bones takes place, osteoporosis in long bones, and symptoms of osteosclerosis
where the bones become denser and develop abnormal crystalline structure. In advanced stages, bones and joints become
weak rendering movement difficult and painful. Fusion of vertebrae is observed
in many areas of the spine. The greatest changes are observed in the
spine, particularly in the cervical region. Kyphosis with limited
spinal mobility, flexion contracture of lower extremities, and restricted chest
wall expansion occur. The “Poker back” spine (kyphosis) is a late
manifestation of skeletal fluorosis wherein the entire spine becomes one
continuous column of bone. In the final stage, the patient is left
crippled. The main mechanism
of skeletal fluorosis is the fluoride incorporation into the bone
hydroxy-apatite, altering the size and structure of its crystals. The
fluorapatite formed decreases the mechanical competence of the bone, resulting
in abnormal structure and poor quality of bone with an increased risk of fractures.
Diving a bit deeper...
Fluoride can
demonstrate biphasic actions (i.e., mitogenic at low concentrations and toxic at
higher concentrations). Fluoride
inhibits a unique fluoride‐sensitive phosphotyrosine phosphatase (PTP) in osteoblasts,
which results in a sustained increase in the tyrosine phosphorylation level of
the key signaling proteins of the MAPK mitogenic transduction pathway, leading
to the potentiation of the bone cell proliferation initiated by growth factors. The fluoride acts in coordination with aluminum to form fluoroaluminate, which
activates a pertussis toxin‐sensitive Gi/o protein on the bone cell membrane, leading to activation of cellular protein tyrosine kinases (PTKs), which in turn leads to
increases in the tyrosine phosphorylation of signaling proteins of the MAPK
mitogenic signal transduction pathway, ultimately leading to a stimulation of
cell proliferation.
Fluoride can act
on osteoblasts and osteoclasts in vivo and in vitro. NaF is an anabolic agent capable of increasing
bone mass, although the mechanism for its action remains unclear. While NaF may
increase bone mass, the newly formed bone appears to lack normal structure and
strength. In trabecular bone, fluoride results in an increase in bone volume
and trabecular thickness without a concomitant increase in trabecular
connectivity. It is this lack of trabecular connectivity that reduces bone
quality despite the increase in bone mass.
All of these explain how fluorosis leads to his skeletal deformity.
Our next question...Can fluorosis somehow increase the chance of renal stone formation?
What we learned from various articles...
The World Health Organization is acutely aware
that fluoride is a kidney toxin, recently citing the finding that approximately
100,000 individuals in the Assam region in India have been taken ill with kidney failure, stiff joints, and anemia as a result of high
natural levels of fluoride in the water [WHO 2015]. Similar results have been
found in other parts of India [Hindu 2017] and Sri Lanka [Dharmaratne 2015].
In another research, 20 urinary stones were taken from patients at a Russian hospital with ion chromatography and conductivity detection. They detected fluoride ions in 80% of the stones, at concentrations of 0.01–4.0mg per gram of stone.
The vast majority of the stones contained very small concentrations of fluorides, below 0.1mg per gram of stone, but two of the stones had fluoride concentrations above 0.5mg. This indicates that the formation of these stones may have been promoted by high concentrations of fluorides in the patients’ urine, perhaps due to the patients ingesting lots of water containing added fluoride or even lots of fluoride toothpaste.[“In our previous experiment using rats, fluoride was reported to cause renal calcification, whose mechanism was deduced to be due to an increase in parathyroid hormone (PTH) secretion. However fluoride-induced renal calcification that was independent of PTH has not been understood well in the nephron of fluoride-treated animals. Thus, we examined the effect of sodium fluoride on intracellular calcium mobilization in a normal rat kidney epithelial cell line (NRK-52E cells). The calcium accumulation was found to be remarkably increased by the addition of sodium fluoride (NaF). The elevation of [Ca2+]i was demonstrated to be due to calcium entry through nifedipine-sensitive calcium channels.”
SOURCE: Murao H, et al. (2000). Sodium fluoride increases intracellular calcium in rat renal epithelial cell line NRK-52E.Biol Pharm Bull. 23(5):581-4.]
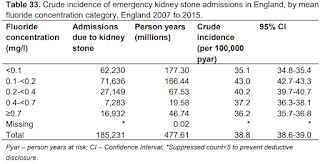
This study shows that there was no
association at higher concentrations, and the test of trend indicated a linear trend was not
present.In another investigation, a case-controlled study was conducted on 824 school children aged 8–15 years, where drinking water
was contaminated with fluoride. This study showed chronic kidney damage to be higher in the affected
children, other than fluorosis, and significantly higher urinary fluoride as
compared to the control area children.Another cross-sectional study conducted on
239 adults (18–77 years old) by monitoring four early kidney injury biomarkers
(ALB, Cys-C, KIM-1, and OPN) related to environmental fluoride exposure,
indicated possible tubular dysfunction due to fluoride exposure, that might
increase susceptibility to the future development of CKD.
The vast majority of the stones contained very small concentrations of fluorides, below 0.1mg per gram of stone, but two of the stones had fluoride concentrations above 0.5mg. This indicates that the formation of these stones may have been promoted by high concentrations of fluorides in the patients’ urine, perhaps due to the patients ingesting lots of water containing added fluoride or even lots of fluoride toothpaste.
SOURCE: Murao H, et al. (2000). Sodium fluoride increases intracellular calcium in rat renal epithelial cell line NRK-52E.Biol Pharm Bull. 23(5):581-4.]
This study shows that there was no association at higher concentrations, and the test of trend indicated a linear trend was not present.























Comments
Post a Comment